Revenue Model
TEAM APPROACH
Medicine is no longer an individual activity. Science has shown that a team approach works better. In addition, population medicine (or denominator medicine) requires a team.
There are many Tom Brady fans in American football. Imagine him winning without a front line protecting him. LeBron James or Micheal Jordan sometimes seemed to "carry the team on their shoulders". But the reality is they needed their team.


Tom Brady has a team. You need one too.
LeBron James or Micheal Jordan sometimes seemed to "carry the team on their shoulders". But the reality is they needed their team.
No matter how good you are in the examination room with your patient, you must have a team protecting you. It would be best if you had a chart review for previous medications, allergies, etc. You need someone reviewing for A1c to ensure that patients have come in for the proper tests at the right time. Even if you are also a certified risk coder, there's no way you can review coding while you're seeing your patient. You cannot do that all alone.
BONUSES - IT'S WHAT A TEAM MEANS FINANCIALLY
It's true that doctors in Value-Based Care programs work fewer hours and typically get paid more. It's because their teams support them. Here are some examples:
AWVs -
Typical bonus programs for AWVs are to initially pay something like $80- $100/AWV. Once you have successfully done AWVs on 80% of that specific payor's patient panel with you, you may go to $150/AWV. But it isn't just those at 80% and above. It goes back to all previous AWVs as well. 90% is another specific cut point for bonus payout. So, as you see, it's not just how well you practice medicine inside the exam room. It's how well your support team can find an get all your patients in the door - & alert you of the need for a specific exam or process. It would help if you had a team of doctors. We've been alone in the exam room with patients as well. We know what you need.
HEDIS -
Payors typically pay for services based on the HEDIS scores of the physician. Many Electronic Medical records claim to track & help you with your HEDIS scores. But CMS calculates your scores based on what they see (successfully billed), not just what's in your EMR.
CAHPS -
CAHPS measures patient & consumer experience, access, timing, clarity & ease of getting care from your team. This is now triple-weighted. You can only achieve financial success in Value-Based care by providing a good patient experience. And you must provide a better experience with a team.
.
HOS -
HOS is triple-weighted. Like CAHPS, triple-weighting makes it critical to achieve financial success.
HOS is the Health Outcome Survey. It's not enough to practice good medicine. You have to achieve the outcomes. That makes it difficult. It requires you & your team to engage the most critical healthcare team member - the patient. How can you engage a patient that has yet to come in unless you know that? That's what we do. We help you with your whole population. That's why they call it population medicine.
5-STAR -
5-STAR is a CMS ranking system separating doctors' performance. The top 20% of doctors are rated 5- STAR and paid the most. It declines with every fewer STAR rating. We're interested, & we need more time to manage 3-STAR, average performers. We're looking for members for a 5-STAR team.
CAPITATION - (PMPM)
Once payors begin to notice your team & your performance, they begin to offer capitation (PMPM - or Per Member Per Month) payments. These are usually adjusted by access, competition, & quality scores. Our Alabama network was offered $30 PMPM early in our start-up based on the team's knowledge & performance. Don't expect to get these offers working alone. Again, you need market penetration, & that requires a team.
RISK-BASED CONTRACTS -
The most financially rewarding arrangements are full-risk. That requires complete function and success in all areas - CAHPS/HOS, HEDIS/5-STAR, Risk Assessment, and full risk management. Expecting to achieve success in all these areas alone is like expecting Tom Brady to win a football game with no front line; it's just not going to happen. We're doctors. We've been there in the exam room. We're experienced in managing all these team components for hundreds of doctors and more than 150,000 patients in 5-STAR, quality-rated, full-risk programs. We're a team of doctors supporting doctors. Please be sure to get the best to support you.
Practical Examples
Group Revenue Analysis
Example 1
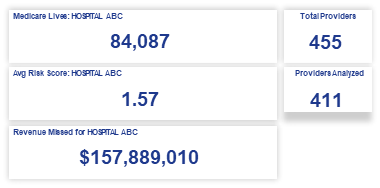
Example 2

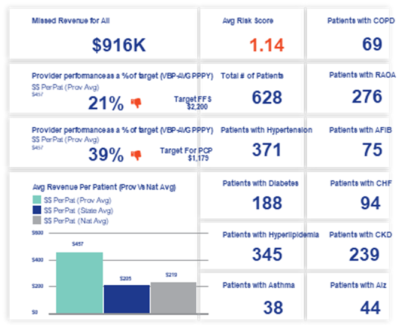
Provider Revenue Analysis
Example 1


Example 2

Sample Early Program: Bonus (“Upside-Only”) 2022 Partnership for Quality (P4Q) Program
The 2022 P4Q Program is upside-only and designed to ensure Cigna Provider Groups/Individual Physicians collaborate to deliver high-quality medical and administrative services for customers.
The 2022 P4Q Program offers four ways for Provider Groups to earn a Quality Incentive Payment.
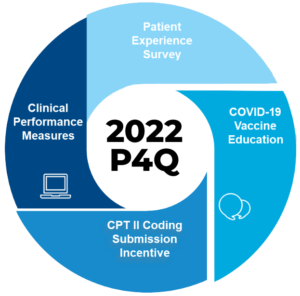
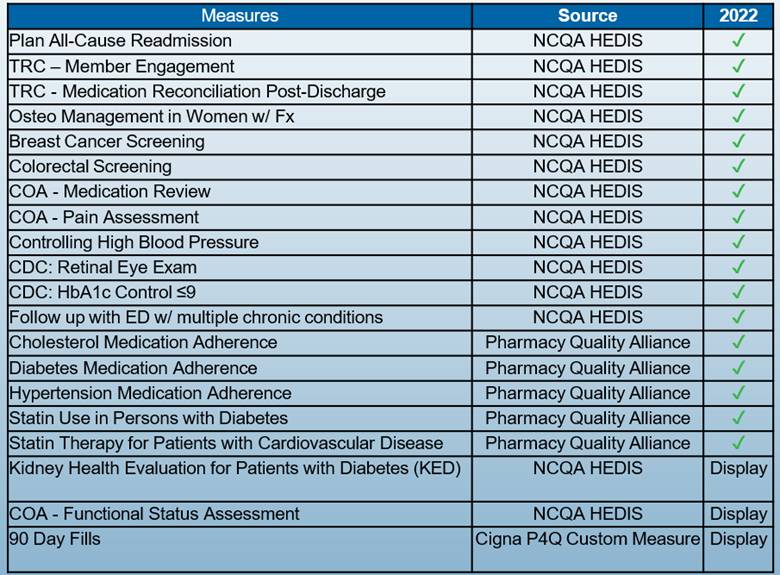
- Clinical Performance Measures align with CMS Stars and are based on CMS, NCQA HEDIS, and Pharmacy Quality Alliance definitions, weights, eligible populations, etc.
- Measures marked “Display” are not a part of the incentive payments; rather, they are monitored by P4Q and provided to participating providers/groups on the P4Q Financial Dashboard for awareness
Sample: Clinical Performance Measures
The completion rate for each Clinical Performance Measure equates to a Star rating
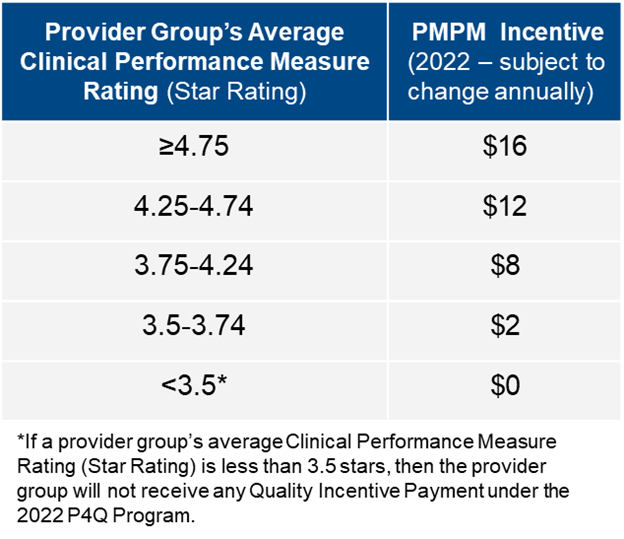
The Provider Group’s Clinical Performance Measure Rating (Star Rating) determines its PMPM incentive rate – see table to the right
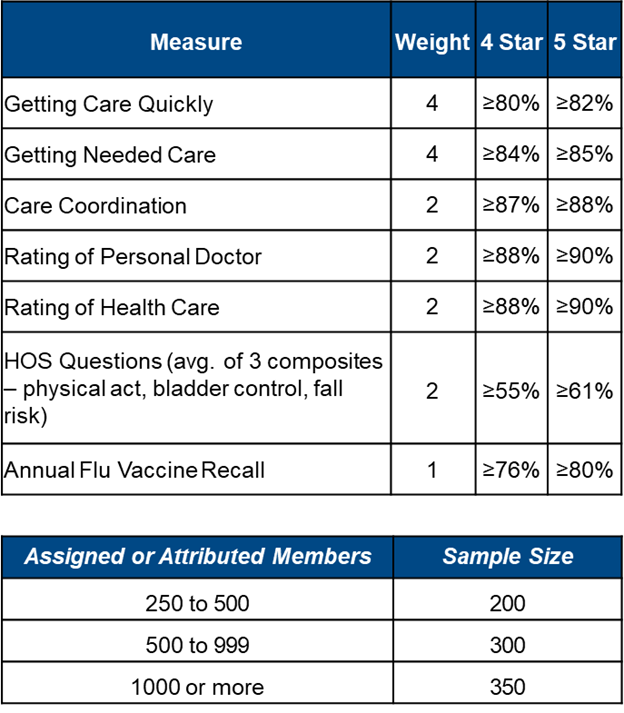
SAMPLE: Experience Surveys
The 2022 P4Q Program allows Provider Groups to earn a Quality Incentive Payment for satisfying Patient Experience Measures aligned with CAHPS and HOS – patient perception and recollection.
Provider Groups that achieve at least a 4 Star rating on the Patient Experience Survey are eligible for an additional Quality Incentive Payment

•Provider Groups must also satisfy the following requirements in order to qualify for the Patient Experience Survey Incentive:
–Provider Group’s Average Clinical Performance Measure Rating is ≥ 3.5
–Provider Group’s collective panel size is ≥ 250 Members
–Sampled Population’s Response Rate ≥ 25%
•Cigna sends the Patient Experience surveys to a random sample of Members based on the number of Assigned or Attributed Members in the collective Provider Group
SAMPLE: Coding Submission Incentive
•The 2022 P4Q Program allows Provider Group to earn a Quality Incentive Payment on a quarterly basis for correctly including CPTII codes on clean claims (paper or electronic) or encounter data submissions.
•The 2022 CPTII Coding Submission Incentive is for the below Clinical Performance Measures, where clinically appropriate (regardless of measure values).
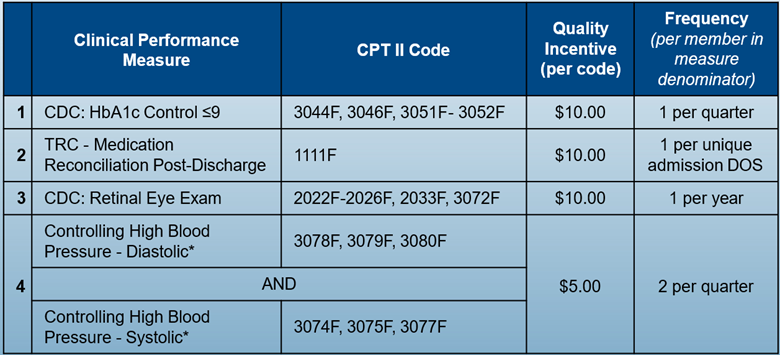
In order to receive the $5.00 CPT II Coding Incentive for Controlling High Blood Pressure, both Diastolic and Systolic CPTII codes must be present for the same date of service.
Ready to find out more?
Call us at 859-721-1414 or email us. Your patients deserve it. Your family deserves it. You deserve it!
